By Nilson Feliz, MD, Manuel Fernandez, MD, Lisa M. Sebastian, MD, Roberto L. Collazo-Maldonado, MD, FACP
A 60-year old African American man was referred for evaluation of nephrotic syndrome. His past medical history was positive for HTN, DM, and Hepatitis C — successfully treated with ombitasvir/periteprevir/dasabuvir for three months. His hepatitis C viral load was undetectable. Upon physical exam, he was hypertensive and had anasarca. Labs showed a creatinine of 2.2 mg/dL (from a baseline of 1.3 mg/dL), serum albumin 1.9 mg/dL, and proteinuria of 11.8 g/day; urine sediment showed 3+ protein with no hematuria or casts, UPIEP showed 35 % M-spike with monoclonal IgG lambda chain and SPIEP showed IgG lambda spike, normal C3 and C4, the remaining serologic evaluation was negative, including cryoglobulins.
He was admitted for IV diuresis, blood pressure control, and work up of his nephrotic syndrome. Skeletal survey was negative. Kidney biopsy showed MPGN on light microscopy with nodular/lobular increases in cells with double contouring, negative cryoglobulins and negative congo red staining, and moderate tubular atrophy. No crescents were seen. EM showed effacement of foot process with basement membrane duplication with subendothelial and subepithelial deposits. IF was positive for IgM and lambda. Bone marrow flow cytometry studies revealed 1% lambda light chain-restricted plasma cells. After discussing the case with a hematologist, we concluded that his MPGN was secondary to MGRS. He was treated with dexamethasone and bortezomib, which showed improvement in creatinine to 1.5 mg/dL and increase in serum albumin to 3.6 mg/dL.
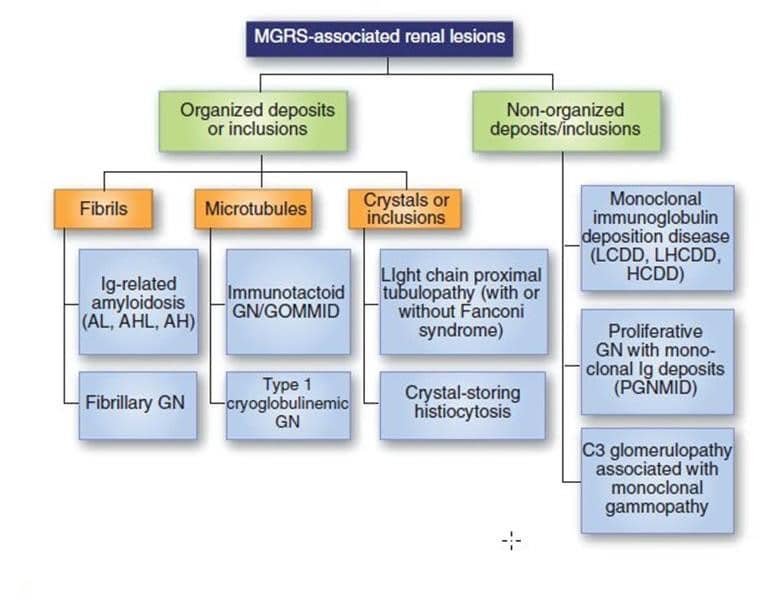
MGRS is a rare cause of membranoproliferative glomerulonephritis (MPGN) due to deposition of monoclonal immunoglobulin complexes in the kidney without the characteristic systemic manifestations of paraproteinemi (see figure). Nephrologists should be aware of this entity and consider it in the differential diagnosis for any patient presenting with elevated creatinine and nephrotic syndrome, and abnormal SPIEP/ UPIEP with no other explanation for renal findings. Collaboration with a hematologist is crucial for diagnosis that can lead to early recognition and treatment.